Our lungs are amazing organs. They help us breathe freely. They are surrounded by a special lining. This lining is called the pleura. Between its layers is a tiny space. This space holds a small amount of fluid. This fluid helps the lungs move smoothly. Sometimes, too much fluid builds up. This condition is pleural effusion. It can be a serious issue. Understanding its causes is key. Diagnosis and treatment vary.
They are surrounded by a special lining.
The pleura has two layers. One layer covers the lung surface. The other lines the chest wall. These layers are very thin. They are smooth and slippery. This design allows for movement. Lungs expand and contract. The pleura prevents friction. It protects the delicate lung tissue. This entire system works harmoniously. Any disruption causes problems. Fluid buildup is one such issue.
This fluid helps the lungs move smoothly.
A small amount of fluid is normal. It acts as a lubricant. This allows the pleura to glide. Imagine two wet panes of glass. They slide easily over each other. This is similar for the lungs. Without this fluid, friction occurs. Breathing would be painful then. The fluid volume is tightly controlled. Production and absorption are balanced. Disruption of this balance leads to problems.
This condition is pleural effusion.
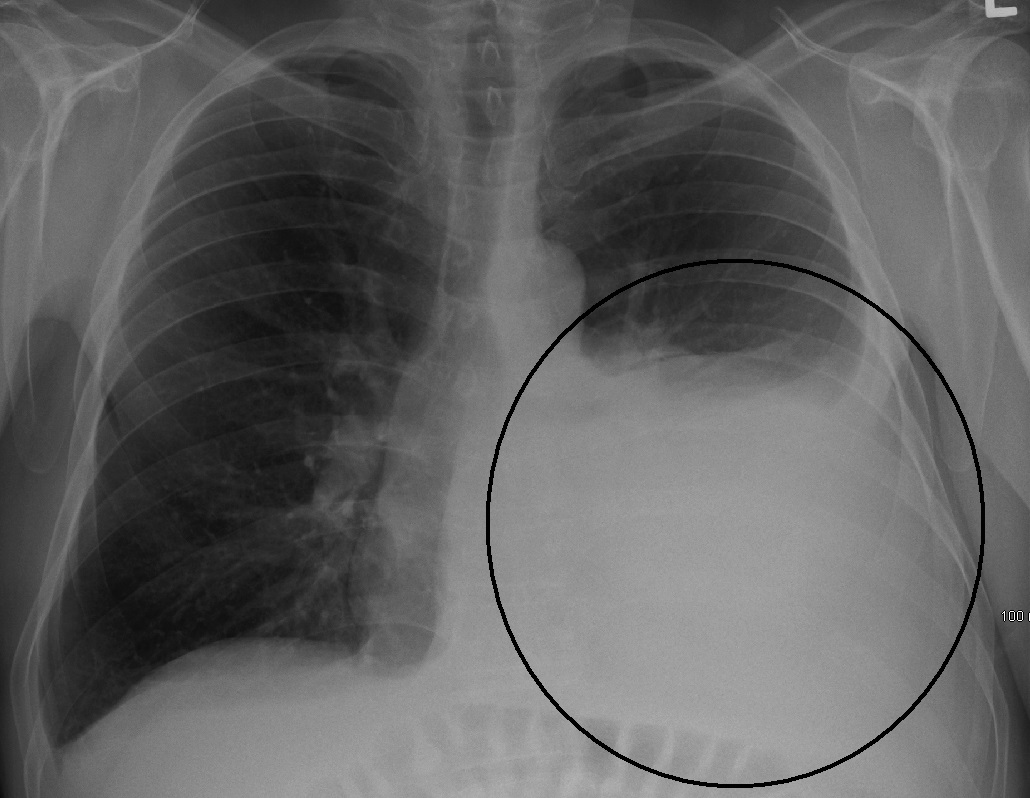
When fluid accumulates, it’s an effusion. The pleural space fills abnormally. This extra fluid presses on the lung. It makes breathing difficult. The lung cannot expand fully. This reduces oxygen intake. Symptoms can range from mild to severe. It’s often a sign of another problem. It rarely occurs on its own. Identifying the root cause is crucial.
“It can be a serious issue.”
A large effusion impacts breathing. It can lead to shortness of breath. The affected lung cannot function well. This puts strain on the heart. It can cause chest pain. It might indicate a severe illness. Cancer can cause effusions. Heart failure is another common reason. Infections like pneumonia are also culprits. Ignoring symptoms is not advisable. Prompt medical attention is vital.
Understanding its causes is key.
Many conditions trigger effusions. Heart failure is a leading cause. Fluid backs up from the heart. Kidney disease can also cause it. Liver cirrhosis leads to fluid retention. Infections like pneumonia are common. Tuberculosis is another infectious cause. Cancer spreading to the pleura is frequent. Autoimmune diseases play a role. Lupus or rheumatoid arthritis are examples. Pulmonary embolism can also be a factor. Each cause has specific implications.
Heart failure is a leading cause.
When the heart struggles, fluid builds. It cannot pump blood efficiently. Pressure increases in blood vessels. Fluid leaks into surrounding tissues. This includes the pleural space. Both sides of the chest can be affected. The fluid is usually clear. It’s called a transudate. This type often signals systemic issues. Treating the heart failure helps. It reduces the fluid accumulation.
Infections like pneumonia are common.
Pneumonia inflames lung tissue. The infection can spread to the pleura. This causes inflammatory fluid. This fluid is usually thick. It contains immune cells and proteins. It’s known as an exudate. It often needs antibiotic treatment. Sometimes, drainage is required. Parapneumonic effusion is specific. It accompanies bacterial pneumonia. Empyema is a severe form. Pus accumulates in the space.
Cancer spreading to the pleura is frequent.
Malignancy often causes effusions. Lung cancer is a common culprit. Breast cancer can also spread there. Ovarian cancer and lymphoma too. Cancer cells irritate the pleura. They cause fluid production. The fluid often contains cancer cells. This is a malignant effusion. It signals advanced disease. Treatment focuses on symptom relief. Palliative care is important.
Autoimmune diseases play a role.
The immune system can mistakenly attack. Lupus can cause pleural inflammation. Rheumatoid arthritis also affects the pleura. These conditions trigger fluid buildup. The fluid is usually an exudate. Treating the autoimmune disease helps. It reduces the inflammation. This in turn reduces the effusion. Management often involves immunosuppressants. It’s part of a broader treatment plan.
Diagnosis and treatment vary.
Doctors start with symptoms. They perform a physical exam. Listening to the chest is key. Imaging tests confirm the fluid. A chest X-ray is often first. Ultrasound helps locate fluid. CT scans provide detailed views. Thoracentesis is a procedure. Fluid is drained for analysis. This helps determine the cause. Treatment then targets the root problem.
They perform a physical exam.
During the exam, doctors listen. They use a stethoscope to listen. Diminished breath sounds suggest fluid. They might hear a pleural rub. This sounds like creaking leather. It indicates inflamed pleural layers. Percussion reveals dullness. Tapping on the chest helps. This dullness means fluid is present. These physical signs guide diagnosis. They point towards potential effusions.
Fluid is drained for analysis.
Thoracentesis is a key step. A needle removes fluid from the chest. This is done carefully by a doctor. Local anesthetic numbs the area. The fluid goes to a lab. They test its protein content. Cell counts are also performed. Glucose and LDH levels are checked. This helps differentiate fluid types. Transudate versus exudate is crucial. It narrows down the possible causes.
This helps determine the cause.
Fluid analysis provides clues. A transudate suggests systemic issues. Heart, kidney, or liver problems are likely. An exudate points to local inflammation. Infection, cancer, or autoimmune disease fit here. Specific cell types indicate causes. Cancer cells confirm malignancy. High white cells suggest infection. This detailed analysis is vital. It guides further investigation.
Treatment then targets the root problem.
Treating the effusion directly helps. But curing the cause is essential. For heart failure, diuretics are given. For infections, antibiotics are used. Cancer treatments vary widely. Immunosuppressants help autoimmune diseases. Sometimes, the fluid is drained. Repeated thoracentesis may be needed. A chest tube might be inserted. This provides continuous drainage.
This provides continuous drainage.
For large or persistent effusions. A chest tube can be inserted. This thin tube goes into the pleural space. It connects to a drainage system. It removes fluid continuously. This helps the lung re-expand. It relieves breathing difficulties. It stays in place for days. Nurses monitor the drainage. It’s a common hospital procedure. It provides significant symptom relief.
It makes breathing difficult.
The fluid takes up space. The lung cannot inflate fully. This reduces lung volume. Oxygen exchange becomes impaired. Patients feel breathless easily. Even at rest, breathing is hard. Physical activity becomes challenging. This significantly impacts daily life. It’s a primary symptom. Relief from this is a main goal. Drainage often provides immediate help.
Ignoring symptoms is not advisable.
Don’t dismiss persistent cough. Don’t ignore shortness of breath. Chest pain should always be checked. These signs warrant medical review. Delaying care can worsen outcomes. The underlying cause might progress. More fluid can accumulate. Complications might develop. Seek professional help promptly. Early detection is always better. It allows for timely intervention.
It allows for timely intervention.
Once diagnosed, steps can be taken. Treatment can begin quickly. This prevents further damage. It improves the patient’s comfort. It can halt disease progression. For severe cases, it can save lives. It offers the best chance for recovery. This emphasizes being proactive. Awareness of symptoms is key. Do not hesitate to consult a doctor.
This is a serious outcome.
Some effusions are life-threatening. Malignant effusions have a poor outlook. Large, rapid accumulations cause distress. They can lead to respiratory failure. Infection can spread widely. Untreated, complications are dire. Understanding the severity is important. It highlights the need for vigilance. It underscores proactive medical care. Every case is unique.
Understanding pleural effusion means recognizing fluid buildup around the lungs, a symptom often indicating underlying conditions that require targeted medical assessment and treatment for relief and improved health.