The transfer of oxygen from the air we breathe to the bloodstream is a fundamental biological process, an exquisite piece of micro-engineering carried out across the vast, thin membranes of the alveoli in the lungs. When we inhale, oxygen rushes into these tiny air sacs, and almost instantly, it diffuses across the delicate alveolar-capillary unit into the waiting red blood cells. The partial pressure of oxygen (PaO2) in the arterial blood must be maintained within a remarkably narrow range to sustain cellular life in all major organs, particularly the brain and heart. Lung diseases, whether acute like pneumonia or chronic like Chronic Obstructive Pulmonary Disease (COPD), systematically dismantle this crucial gas exchange mechanism. They introduce structural barriers, alter ventilation dynamics, or redirect blood flow, all of which lead to hypoxemia, the clinical term for abnormally low oxygen levels in the arterial blood. Understanding the full scope of this impact requires moving beyond the simple idea of “difficulty breathing” to examine the distinct physiological pathways by which pulmonary pathology creates an oxygen deficit in the circulatory system, a failure that cascades into a systemic energy crisis for the entire body. The mechanisms are complex and often intertwined, creating a challenge for clinicians attempting to restore homeostasis.
They introduce structural barriers, alter ventilation dynamics, or redirect blood flow, all of which lead to hypoxemia.
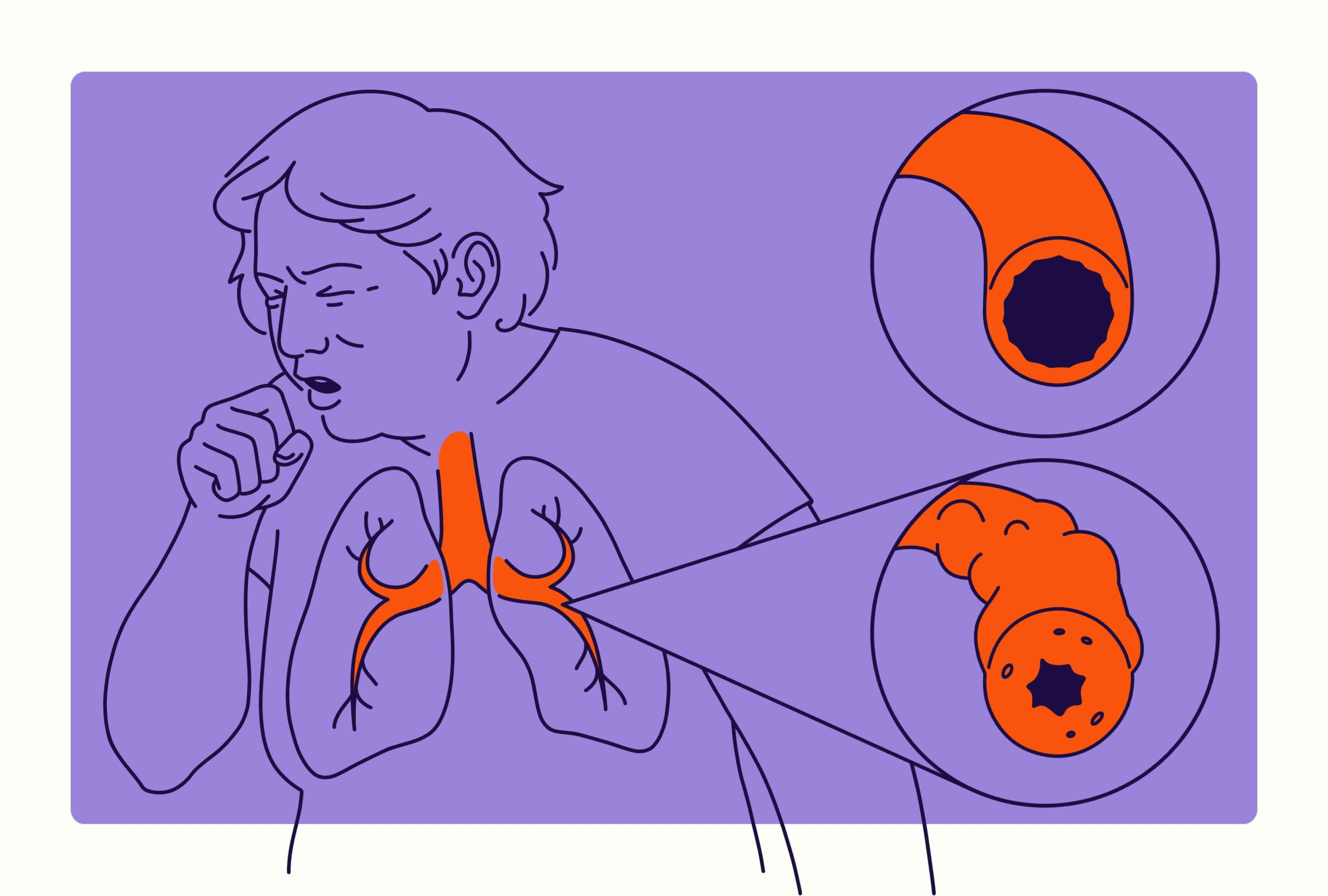
The most pervasive and complex cause of hypoxemia in nearly all lung diseases is the ventilation-perfusion (V/Q) mismatch. For oxygen to efficiently enter the blood, there must be a harmonious balance between the amount of air, or ventilation (V), reaching the alveoli and the amount of blood, or perfusion (Q), flowing through the capillaries that surround them. Ideally, the V/Q ratio should be close to 0.8. However, when lung tissue becomes diseased, this ratio is thrown into disarray. In conditions like emphysema (a form of COPD), the destruction of the alveolar walls and surrounding capillary beds leads to areas where there is adequate air but very little blood flow; this is known as a high V/Q ratio, or alveolar dead space. Conversely, in conditions like asthma or chronic bronchitis, inflammation and bronchoconstriction lead to narrowed airways and mucus plugging, meaning blood flows to lung units that receive very little air; this is a low V/Q ratio, or shunt-like effect. Blood passing through these poorly ventilated areas returns to the left side of the heart still deoxygenated, dragging the overall arterial oxygen content down and proving notoriously resistant to correction with simple supplemental oxygen.
The most pervasive and complex cause of hypoxemia in nearly all lung diseases is the ventilation-perfusion (V/Q) mismatch.
Beyond the problem of airflow distribution, some diseases specifically target the physical barrier between air and blood, causing diffusion impairment. This mechanism is particularly pronounced in Interstitial Lung Diseases (ILDs), such as pulmonary fibrosis. In a healthy lung, the alveolar-capillary membrane is extraordinarily thin—sometimes less than one micron—allowing oxygen molecules to effortlessly “diffuse” across into the blood. In pulmonary fibrosis, chronic inflammation leads to the deposition of scar tissue and fibrosis around the alveoli and within the interstitial space. This scarring creates a thickened, inflexible barrier that oxygen must struggle to cross. While gas exchange might appear normal at rest, the problem is dramatically exposed during physical exertion. When a person exercises, blood rushes through the pulmonary capillaries faster, reducing the time that the red blood cells spend near the alveoli. Because of the thickened barrier, the oxygen now requires more time to diffuse, and the short transit time means the blood leaves the lungs before it can be fully saturated. This is why individuals with severe ILD often experience a profound, activity-dependent drop in their blood oxygen saturation.
This scarring creates a thickened, inflexible barrier that oxygen must struggle to cross.
An even more extreme version of the V/Q mismatch is the true pulmonary shunt, where deoxygenated blood bypasses functional alveoli entirely. This is a common and dangerous mechanism in acute, severe conditions like Acute Respiratory Distress Syndrome (ARDS) or severe pneumonia. In these diseases, the alveoli fill up completely with fluid, pus, or cellular debris, known as intra-alveolar exudates. The affected areas are completely cut off from ventilation, rendering the air sacs non-functional. However, the blood vessels surrounding these flooded alveoli remain perfused. Blood flows past these collapsed or fluid-filled units without picking up any oxygen and, crucially, without being directed away by the body’s usual protective reflex known as hypoxic pulmonary vasoconstriction (HPV). Since this blood is never exposed to air, the resultant drop in arterial oxygen is profound. Unlike hypoxemia caused by simple mismatch, the oxygen deficit caused by a true shunt responds very poorly to increasing the concentration of inhaled oxygen, because the supplemental oxygen can’t even reach the blood.
This blood is never exposed to air, the resultant drop in arterial oxygen is profound.
In many advanced lung diseases, particularly severe COPD and conditions that affect the respiratory muscles or neurological control, the problem lies not in the lung’s structure, but in the total amount of air exchanged, a state called hypoventilation. This occurs when the overall breathing rate is too slow or too shallow to meet the body’s metabolic demands. In COPD, the chronic retention of air due to airway obstruction effectively limits the fresh air that can enter the lungs, meaning the alveolar air has a lower partial pressure of oxygen and, simultaneously, a dangerously high concentration of carbon dioxide (PaCO2). As the total alveolar pressure is relatively constant, an increase in PaCO2 forces a proportional decrease in alveolar oxygen tension (PAO2), leading directly to a lower oxygen level in the arterial blood. This is a critical distinction, as hypoxemia caused solely by hypoventilation can often be readily corrected by increasing the percentage of inhaled oxygen, but it frequently comes at the risk of worsening carbon dioxide retention, a delicate clinical balancing act.
This occurs when the overall breathing rate is too slow or too shallow to meet the body’s metabolic demands.
The systemic impact of chronic oxygen deprivation extends into the pulmonary vasculature itself, generating a vicious cycle of disease. Prolonged hypoxemia—specifically the low oxygen tension within the alveoli—triggers a localized defense mechanism known as hypoxic pulmonary vasoconstriction (HPV), which attempts to divert blood away from poorly ventilated lung areas. However, when large areas of the lung are chronically hypoxic, this widespread and sustained vasoconstriction leads to a pathological increase in the mean pressure within the pulmonary arteries, a condition known as pulmonary hypertension (PH). This elevated pressure forces the delicate vascular walls to thicken and remodel structurally, making the hypertension permanent and irreversible in advanced cases. The added workload eventually strains the right ventricle of the heart, which is responsible for pumping blood into the lungs. This progressive failure of the right side of the heart due to lung disease is medically termed Cor Pulmonale, a severe, life-threatening consequence where the body’s primary pump fails because of the lung’s inability to properly oxygenate the blood.
Prolonged hypoxemia—specifically the low oxygen tension within the alveoli—triggers a localized defense mechanism known as hypoxic pulmonary vasoconstriction (HPV).
The consequences of low blood oxygen are not merely confined to breathing difficulties; they represent a fundamental threat to systemic organ function, reflecting the pervasive need for a steady oxygen supply. When PaO2 drops significantly, the central nervous system, which has the highest oxygen demand of any organ, begins to suffer. Symptoms of hypoxemia in its severe form often present as neurological disturbances, including confusion, disorientation, and impaired judgment. This makes even simple tasks incredibly dangerous for a patient. Furthermore, the heart, in a desperate attempt to compensate for the insufficient oxygen supply, increases its output, resulting in a rapid heart rate (tachycardia). Over time, this chronic overexertion can lead to heart rhythm abnormalities or outright heart failure. The visible signs of this systemic crisis, such as the bluish discoloration of the skin, lips, and nail beds (cyanosis), are a late and serious indicator that the body’s hemoglobin is failing to deliver its critical cargo.
The visible signs of this systemic crisis, such as the bluish discoloration of the skin, lips, and nail beds (cyanosis), are a late and serious indicator.
The intricate relationship between chronic lung disease and sleep creates a separate but significant pathology known as nocturnal hypoxemia. During sleep, everyone experiences a natural, minor drop in their respiratory drive and, consequently, a slight decrease in oxygen saturation. However, in individuals with existing lung conditions like COPD or obstructive sleep apnea (OSA), this normal physiological dip is exaggerated and can become acutely dangerous. Periods of interrupted or shallow breathing during the deepest stages of sleep cause oxygen levels to plummet repeatedly throughout the night. This repeated desaturation not only deprives the brain and body of rest but also dramatically exacerbates the underlying pulmonary hypertension. This cycle of recurrent nocturnal oxygen deficiency is a powerful, silent driver of disease progression, often contributing to morning headaches, profound fatigue, and worsening daytime gas exchange efficiency. Addressing these nighttime dips with continuous positive airway pressure (CPAP) or supplemental oxygen is often one of the most effective interventions to slow disease progression and improve quality of life.
The intricate relationship between chronic lung disease and sleep creates a separate but significant pathology known as nocturnal hypoxemia.
The distinction between how different pulmonary diseases impact blood gas parameters is critical for accurate diagnosis and management. For instance, in conditions dominated by pulmonary shunt (like severe pneumonia), the Alveolar-Arterial (A-a) oxygen gradient is significantly widened, indicating a large discrepancy between the oxygen concentration in the alveoli and the final concentration achieved in the arterial blood, a classic sign of impaired oxygen transfer that is not readily fixed by increasing inspired O2. Conversely, in hypoxemia caused purely by hypoventilation (such as from a drug overdose affecting the respiratory drive), the A-a gradient remains relatively normal, because the low oxygen is a systemic failure of breathing rather than a localized lung defect. Clinical intervention, therefore, differs drastically: a widened gradient mandates aggressive lung treatment, while a normal gradient directs therapy toward restoring the body’s mechanical or neurological breathing function. This diagnostic step avoids blindly administering oxygen, which could be ineffective or even counterproductive in specific contexts.
This diagnostic step avoids blindly administering oxygen, which could be ineffective or even counterproductive in specific contexts.
Therapeutic interventions to raise blood oxygen levels must directly address the underlying mechanism of hypoxemia, moving beyond the mere delivery of supplemental oxygen. In cases where the problem is obstructive (like COPD or severe asthma), the primary goal is to physically open the airways using bronchodilators and reduce inflammation with corticosteroids, allowing for better ventilation and thus improving the V/Q balance. For diseases characterized by widespread fibrosis or diffusion impairment (like ILD), the focus shifts to anti-fibrotic medications to halt the structural remodeling, alongside high-flow oxygen delivery to overcome the thickened barrier by maximizing the diffusion gradient. When severe respiratory failure sets in, non-invasive or invasive mechanical ventilation is required not only to supply oxygen but, more importantly, to help expel the retained CO2 and physically recruit collapsed alveolar units, effectively acting as an external lung to buy time for the body to heal. The oxygenation strategy is, therefore, a highly nuanced approach tailored to the specific pathology driving the oxygen deficit.
Therapeutic interventions to raise blood oxygen levels must directly address the underlying mechanism of hypoxemia, moving beyond the mere delivery of supplemental oxygen.
The long-term effects of chronic, low-level hypoxemia extend far beyond the lung-heart axis, silently influencing a patient’s entire metabolic profile and overall longevity. One often overlooked consequence is the body’s attempt to adapt by stimulating the production of more red blood cells, a condition known as secondary polycythemia. This is an attempt to increase the blood’s total oxygen-carrying capacity. While seemingly adaptive, this increase in red cell mass also raises the viscosity (thickness) of the blood. Thicker blood requires the heart to work harder to pump it through the pulmonary and systemic circulation, adding further strain to an already compromised cardiovascular system and increasing the risk of potentially fatal complications, such as thrombotic events or stroke. The continuous state of oxygen scarcity effectively ages the body’s organ systems prematurely, diminishing overall physiological reserve and explaining the complex array of non-respiratory symptoms—from chronic fatigue to muscle wasting—that burden individuals living with advanced lung disease.